SRI has created a novel platform that could significantly expand the benefit of immunotherapies by “infecting” cancer cells
By: Indu Venugopal, Ph.D., Research Scientist, SRI International
The human immune system acts as a precision military force, seeking out and eliminating foreign invaders such as viruses, bacteria and even cancer cells. Unfortunately, at times, this force can be outmaneuvered or even overwhelmed, and the invaders can take over.
In the case of cancer, researchers have created powerful new therapies that help to stimulate and reinforce the immune system, adding soldiers to the fight. Given their effectiveness, these immunotherapies are quickly emerging as first-line treatment for multiple types of cancer. While they’ve contributed significantly to some patients’ survival, these therapies also have limitations. In addition to high cost and potentially serious side effects, they work only for a specific and still fairly limited group of patients.
Our team at SRI has developed a new immunotherapy with the potential to overcome these challenges and extend the benefits of immunotherapy to many more patients. How did we do it? Essentially, we’ve developed a way to make cancer cells look like they have the measles, encouraging the human immune system to seek out and kill an invader it already knows how to fight.
Outfoxing a key drug discovery challenge
The basis for this discovery is a novel SRI platform called the FOX Three Molecular Guidance System (MGS)™. We created FOX Three to solve another critical drug development challenge — delivering potential new therapies into targeted cells to treat disease. Many molecular compounds are just too large to get into cells and therefore make the targets inside those cells “undruggable.”
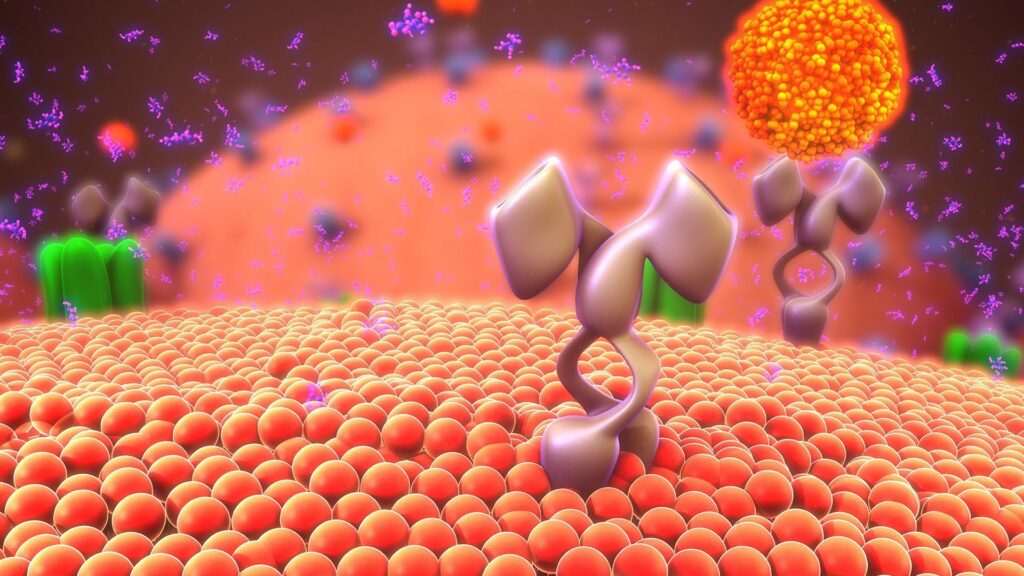
The FOX Three platform rapidly and systematically identifies small chains of amino acids (i.e., peptides), which we call Molecular Guidance Systems (MGS), that serve as unique therapeutic delivery agents. When attached to a specific therapeutic payload such as a monoclonal antibody or siRNA, these agents home and bind to the targeted cell type and then trigger the cell to internalize the cargo.
Using the FOX Three platform, we’ve now developed a unique new immunotherapy. This approach, which we call Targeted Antigen Loaded Liposomes (TALL), has demonstrated potential to help the 80 percent of cancer patients who currently don’t respond to checkpoint inhibitors (CKIs), the leading category of cancer immunotherapies.
Helping the immune system recognize and kill cancer cells
TALL is almost unfairly tricky. It works like this: We pack a synthetic peptide derived from the measles virus into a neutral stealth particle known as a liposome. We then attach tumor-targeting MGSs to the surface of the liposome. The MGSs home to tumor cells and, once there, the liposomes are transported into them. Following some internal workings, the cell presents the measles peptide antigen on its surface. These antigens serve as an alert to the immune system — a molecular “red flag” if you will — signifying a foreign body or substance. For all intents and purposes, the cancer cells now look to the immune system as if they are “infected” with measles.
The vast majority of humans worldwide have been vaccinated for measles, so the immune system already recognizes this invader and is primed to respond to it; when TALL peptides infiltrate the cancer cells and attach their biological red flags, immune cells flood into the tumor environment and begin killing those cells. And because this therapy only flags tumor cells, it leaves healthy cells untouched, reducing the potential for serious side effects.
In pre-clinical research, TALL generated the anticipated actions: Liposomes accumulated in targeted cancer cells and the cells were subsequently flagged with measle peptide. This generated a rapid and robust immune system response against the targeted tumor cells and a significant reduction in tumor growth.
Additionally, early research suggests that the TALL system could greatly expand the benefits of existing immunotherapies, including CKIs. These drugs are rapidly becoming standard of care for many cancer types because — in those cancers that are readily recognized by the immune system and generate a significant immune response — they are very effective. Unfortunately, about 80 percent of cancers don’t naturally generate a significant immune system reaction. CKIs are far less effective in these patients.
By getting the immune system to more readily recognize these cancers — i.e., calling attention to them — TALL can overcome this drawback. In a pre-clinical study looking at an aggressive type of breast cancer, combining TALL with a leading CKI led to a 93 percent reduction in tumor volumes as compared to using CKI alone. Based on these and other recent findings, we are hopeful that TALL will provide a powerful new immune system ally in the fight against cancer.